GM case discussion
This is is an online E log book to discuss our patient's deidentified health data shared after taking his/her/guardian's signed in formed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence-based inputs.This e-log book also reflects my patient centered online learning protfolio and your valuable inputs on comment box is welcome.
A 42 year old male patient resident of choutuppal came to the hospital with cheif complaints of pain abdomen since yesterday
and vomitings since today morning
History of present illness
Patient was apparently asymptomatic 1day back then he developed pain during night after taking meals initially pain is moderate at night then pain became severe at morning 4:00am after vomitings and brought to hospital
pain is in epigastric region which is sudden in onset gradually progressive dragging type radiating towards back relieved on leaning forward aggravated after vomiting
Vomitings started at morning which is non-projectile and bilious 8 episodes of vomiting from morning to evening
H/O of low grade fever is present
H/O of alcohol consumption 3days back
Patient again consuming alcohol since 8months daily 2 bottles of beer after stoppage of 3years
No H/O of constipation and diarrhea
No H/O of abdominal distension
Past history
History of Similar complaints 4 years back where is developed abdominal pain and distension and stopped consumption of alcohol as suggested by doctor
N/K/C/O HTN, Diabetes,epilepsy,TB,asthma
Personal history
• Diet : mixed
• Appetite: normal
• Sleep : distributed if alcohol is not consumed
• Bowel habits: normal
• Bladder habits : normal
Addictions :Alcohol consumption since 16 years and tobacco since 4years
Family history
NO H/O HTN, Diabetes,epilepsy,TB,asthma
Physical examination
General examination
Patient conscious coherent and well oriented to place and time
• Pallor is present
• No Icterus is present
• No cyanosis
• No lymphadenopathy
• No clubbing of fingers
• Moderately built and moderately nourished
Vitals
Temperature: Afebrile
Pulse rate: 66/min
BP: 120/70mm of Hg
RR:12cycles per min
SYSTEMIC EXAMINATION
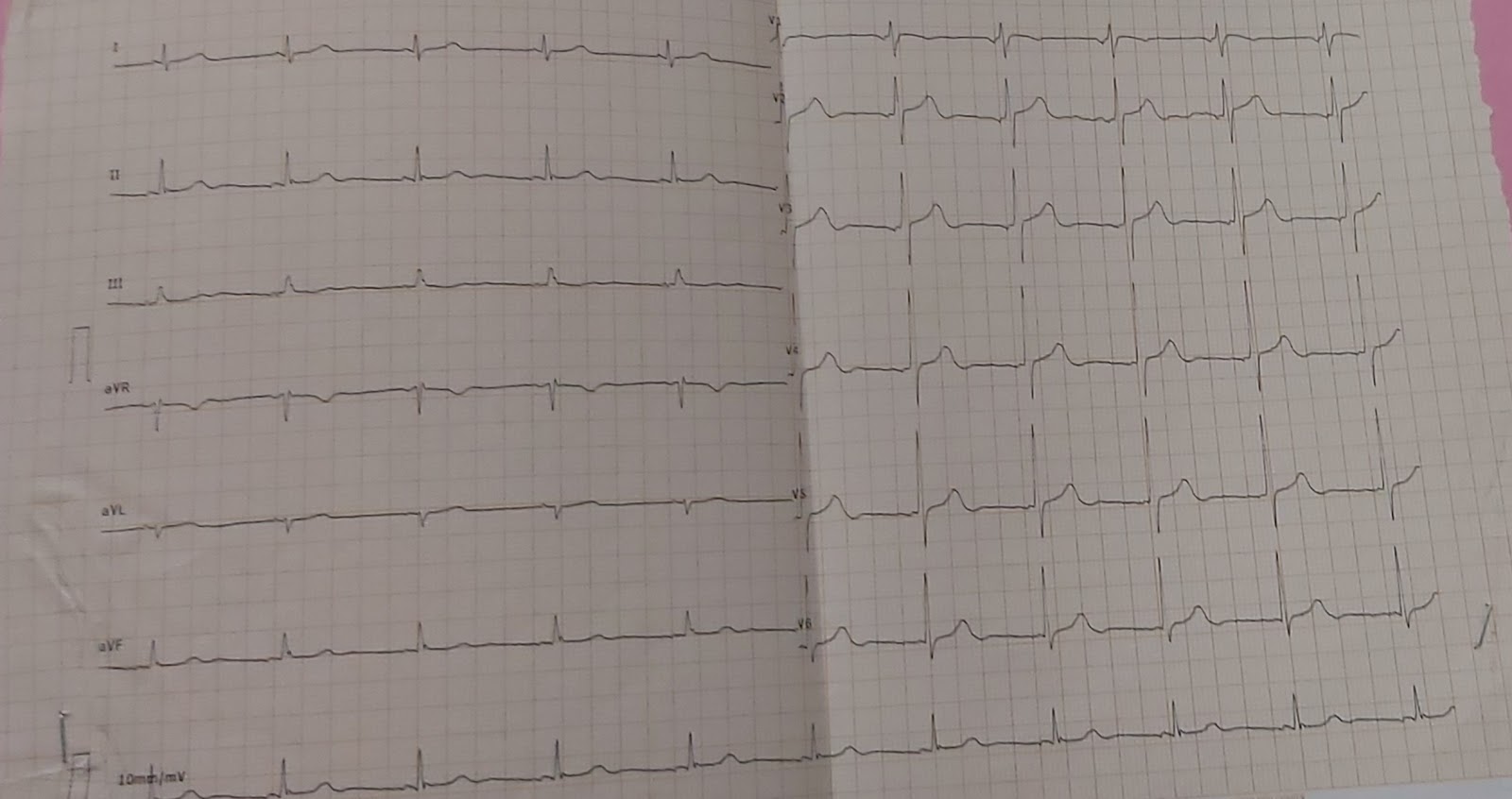
CVS
S1,S2 Heard
No murmurs
RESPIRATORY SYSTEM
No Dyspnea
No wheezes
Trachea-Central
Breath sounds-vesicular
ABDOMEN
Tenderness present in epigastric region
Guarding is present
No palpable mass
No free fluid
No palpable spleen and liver
CNS
Conscious
Coherent
Cooperative
Speech-normal
No neck stiffness
Sensory system- Normal
Motor system- normal
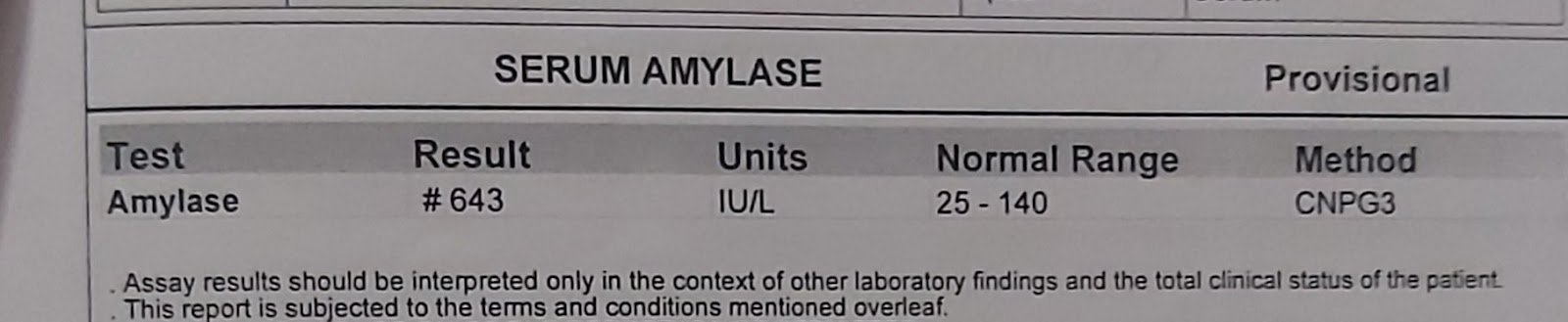
Provisional diagnosis: Acute pancreatitis secondary to alcohol abuse
Investigations







Comments
Post a Comment